Introduction
Telemedicine is used to deliver healthcare from a distance through telecommunication and electronic information. The use of telehealth for neurology consultations, both general and subspecialty, has been shown to be promising.1–3 Various studies have evaluated the safety and efficacy of telemedicine in determining neurological diagnoses.4,5 Telemedicine consultations have been reported to be as effective and safe as in-person consultations. Specifically for headaches, a review examining the comparability of telehealth and in-person consultations for patients with non-acute headaches found no significant differences in outcomes, including treatment efficacy, changes in headache status, severity, and long-term results.6
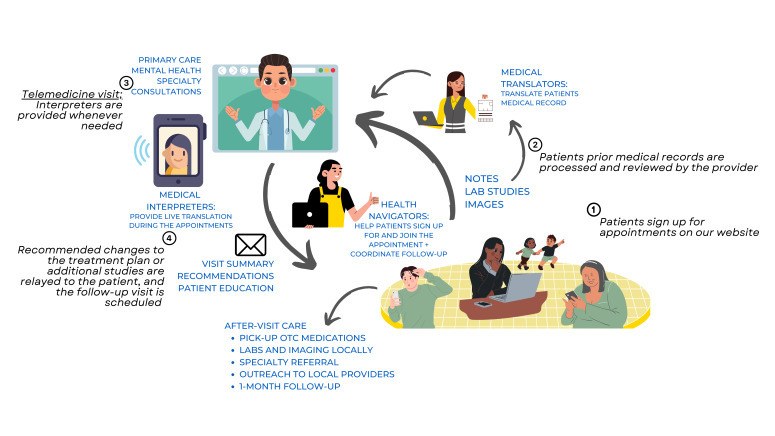
Telemedicine is widely utilized in neurology to provide treatment for a range of conditions like headache and stroke, including in regions of humanitarian crises when access to in-person evaluation is limited. TeleHelp Ukraine, a nonprofit 501c3 charity, offers free medical consultations to Ukrainians affected by the Russian invasion, including neurology care. This case report provides a summary of how a diagnosis of hemicrania continua was determined – and successful treatment was guided – via the TeleHelp Ukraine telemedicine workflow.7
TeleHelp Ukraine (THU) operates using a coordinated workflow involving online appointment scheduling, multilingual interpreters, and a network of volunteer providers across specialties to deliver telemedicine care to displaced Ukrainians during the war, ensuring accessibility despite language and geographic barriers. The figure shown above is the same figure originally published in the cited paper, illustrating THU’s core workflow.7
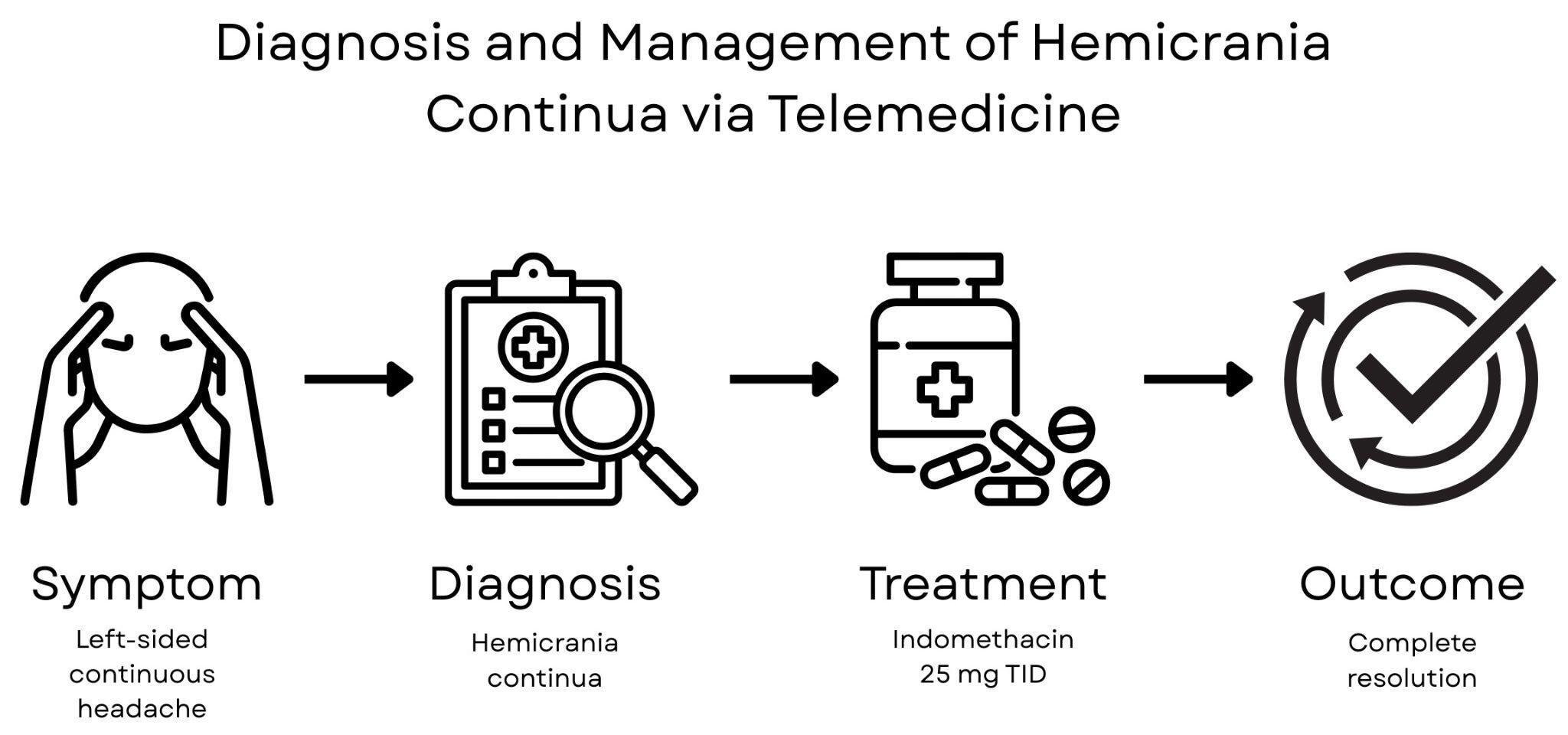
We present a case demonstrating how telemedicine enabled the diagnosis and successful management of hemicrania continua during the ongoing conflict in Ukraine.
Case Presentation
Patient Information
A 52-year-old woman living in Ukraine with a pertinent medical history of dyslipidemia and chronic left internal carotid artery (ICA) occlusion presented for a telemedicine evaluation of a left-sided hemicranial headache lasting two years. She had been previously under the care of local neurologists, but disruptions in services due to Russian air strikes prevented her from following up with in-person medical care.
Clinical Findings
The patient described the headaches as severe, throbbing, retro-orbital, and radiating to the left mandible, maxilla, neck, and shoulder. The pain was daily, constant, non-pulsatile, and non-lancinating, associated with subjective facial swelling, lacrimation, and ptosis but no miosis or anhidrosis. She denied previous strokes, weight loss, or neurological deficits related to the headaches. She also reported stable right-sided cervical lymphadenopathy noted for several years.
Prior in-person evaluations by multiple neurologists in Ukraine included trials of lornoxicam, gabapentin, pregabalin, lamotrigine, and chlorprothixene, none of which relieved symptoms. She was also started on low-dose aspirin and atorvastatin for carotid artery disease but discontinued atorvastatin due to nausea.
Timeline
Diagnostic Assessment
A previously obtained CT angiogram of her head and neck demonstrated complete occlusion (100%) of the left internal carotid artery just 9 mm distal to the bifurcation, without reconstitution of blood flow distal to the occlusion and with no mention of vascular wall compromise such as would be seen in a case of carotid dissection. The left hemisphere arteries showed reduced contrast intensity and diameter compared to the right. The circle of Willis was incomplete, lacking posterior communicating arteries.8 There was also evidence of chronic sinusitis and right-sided cervical and mediastinal lymphadenopathy.
Brain MRI was unremarkable aside from nonspecific white matter changes. MRI of the cervical spine showed protrusions of intervertebral discs at C5-6 and C6-7, degenerative stenosis of the spinal canal at those levels, spondylo-arthrosis, spondylosis, and cystic-solid formations of the soft tissues in the neck, none considered contributory to her headache symptoms.
Therapeutic Intervention
Empirical treatment with indomethacin was initiated remotely via telemedicine. Most patients with hemicrania continua experience pain relief within 24 to 48 hours, but up to 10 days of treatment may be required for effect.9–12 After 3 days of indomethacin 25 mg TID, the patient reported complete resolution of her symptoms. It is unknown how the patient obtained indomethacin, as access to medications can be challenging in conflict zones. Local pharmacies appear to remain functional in her area, and telemedicine platforms such as TeleHelp Ukraine facilitate prescribing and treatment access, overcoming barriers created by disrupted healthcare services.7
Follow-up and Outcomes
At follow-up, the patient remained asymptomatic and reported substantial improvement in quality of life. She expressed gratitude for telemedicine access, stating that without it, she would have had no access to specialized neurological evaluation during the war.
Discussion
Hemicrania continua is a chronic and persistent headache characterized by one-sided, continuous pain that may fluctuate in intensity throughout the day.9,10 In contrast, paroxysmal hemicrania presents with short, intermittent attacks of severe pain, typically lasting 2 to 30 minutes and occurring multiple times per day.13 This distinction is important for accurate diagnosis and management. Our patient’s headache was continuous, consistent with the presentation of hemicrania continua rather than paroxysmal hemicrania.9,10,13 Both conditions may be associated with autonomic features, including ipsilateral facial sweating, nasal congestion, rhinorrhea, tearing, conjunctival injection, eyelid edema, miosis, and ptosis.10
Hemicrania continua is a primary headache disorder and a type of trigeminal autonomic cephalalgia (TAC). It differs from other TACs in that it is characterized by a continuous background headache.14 Classical presentation includes a daily headache of moderate intensity on the same side with intermittent short, piercing pains lasting months. Diagnostic criteria include responsiveness to treatment with indomethacin, a nonsteroidal anti-inflammatory drug (NSAID). This does not appear to be a class effect, as hemicrania continua responds poorly to other NSAIDs for reasons still not understood.9–12
Regarding the chronic left ICA occlusion, it is important to clarify that an occlusion is defined as a complete (100%) blockage, with no partial degrees. The patient’s imaging confirmed total occlusion of the left ICA with no distal reconstitution. While revascularization is recommended for symptomatic carotid stenosis ≥70–80%, especially when associated with ischemic symptoms, complete occlusions without neurological deficits or cerebral ischemia generally do not benefit from revascularization and are managed conservatively.8 In this case, the patient’s headache was attributed to a primary headache disorder unrelated to the vascular occlusion.
A brain MRI and cervical spine MRI showed nonspecific changes but no secondary causes of headache warranting surgical or vascular intervention.
Telemedicine Implications
Telemedicine successfully enabled the diagnosis and management of hemicrania continua despite the conflict-related healthcare disruption. This case highlights telemedicine’s critical role in delivering specialty neurology care when in-person access is limited.15–17
Limitations
Limitations of telemedicine include the inability to perform detailed physical exams such as auscultation for carotid bruits and the challenge of verifying medication acquisition. Despite these, teleneurology has been shown to be effective for headache management, often providing comparable outcomes to in-person care.4–6,18 The American Headache Society notes headache patients require more frequent remote consultations than other neurology patients, underscoring telemedicine’s role.19
The ongoing war in Ukraine has strained healthcare infrastructure, causing shortages of staff, medicines, and supplies. Telemedicine platforms like TeleHelp Ukraine provide vital continuity of care for displaced and underserved patients.20–24
Patient Perspective
The patient reported that telemedicine enabled her to finally receive effective treatment after years of pain. She expressed relief at being able to access care in her native language despite ongoing regional instability.
Conclusion and Learning Points
Telemedicine can facilitate accurate diagnosis and management of complex neurological disorders, including rare primary headaches, even in crisis-affected settings.
Key Learning Points
-
Hemicrania continua should be considered in patients with continuous, unilateral headaches responsive to indomethacin.
-
Telemedicine offers a feasible and effective platform for neurological diagnosis and management in humanitarian and resource-limited contexts.
-
Structured workflows, interpreters, and local pharmacy collaboration are essential for sustaining care during crises.
Ethics Statement
Informed consent was obtained from the patient for publication of this case report and accompanying data, in accordance with the CARE guidelines. Ethical approval was not required as this is a single-patient case report.
Conflict of Interest Statement
The authors declare no conflicts of interest.
Funding Statement
No external funding was received for this work.