1.0 INTRODUCTION
The last two decades have documented changing demographic patterns as never witnessed before with an increasing number and proportion of older persons (aged 60 years and older) across the world.1 By the year 2025, the world will record 1.2 billion people aged 60 years and older and by 2050, it is estimated to increase to over 2 billion with 80% of this population living in low- and middle-income countries.1–3 In sub-Saharan Africa, the rise in the number of older persons is predicted to be the second fastest rate after Eastern and South-Eastern Asia.4 Nigeria has the largest aging population in sub-Saharan Africa and is projected to increase from over 9 million in 2016 to 26 million by 2050.5–7
However, in the last four decades, the northern part of Nigeria has suffered recurrent armed conflicts with consequent impact on people of all age groups including older persons.8 In north central Nigeria, Plateau state was one of the states badly affected in the early years of these conflicts and within this state, Riyom Local Government Area (L.G.A) was one of the worst hit communities.9 The effect of armed conflicts and its attendant consequences on an individual or group can lead to mental health conditions such as depression among others.10
Depression is a public health concern of global dimensions and presently the leading cause of disability worldwide and a major contributor to the overall global burden of disease.1,11 About 5.0% of adults across the world suffer from depression,12 and among older persons it is prevalent as one of the common mental disorders in old age.13 In older persons, the global prevalence of depression ranges from 7.2 to 20%.14,15 This wide range might represent problems with a threshold cut-off for clinical depression in several studies. Apart from this, there is accumulating evidence of subthreshold forms of depression among the older persons which are associated with functional impairments and based on these studies, several authors have argued that categorical approach to clinical depression could be difficult to apply in older persons who have co-occurring health problems.16–18 In view of this, dimensional approach to depression recognition among the elderly is suggested to reduce the gap of older persons with depression who do not receive medical care because they fall short of clinical diagnosis.16
Depression or its symptoms has been identified as a disabling condition that increases the risk of mortality and negatively influences quality of life (QOL).19 The concept of QOL as defined by World Health Organisation (WHO) refers to ‘individuals’ perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns’.20 Late life is a period fraught with frailty, structural and functional deficits heightened by the normal aging process and deteriorating health conditions. Geriatric depression amplifies these disabilities, and if left unattended may become chronic with consequent health and socioeconomic losses impacting negatively on their QOL.13,21
Literature examining depression in late life and QOL of the older persons are increasing but few studies have been conducted on internally displaced older persons in rural communities in Africa. Largely understudied is sub-threshold depression among these persons who have experienced catastrophic events especially in sub-Saharan Africa. While this study estimated the prevalence of major and sub-threshold depression among this population, it also tested the alternative hypothesis that full and sub-threshold depression would have negative effects on the QOL of internally displaced older adults. Thus it builds on the existing evidence that late life depression has negative association with QOL.
2.0 METHODS
2.1 Study design and sample
A community based cross sectional study was conducted among older persons in Riyom Local Government Area of Plateau state, Nigeria. Participants were recruited using a multistage sampling technique, comprising the selection of a L.G.A; community; houses, and eligible participants. The study population comprised internally displaced older adults aged 60 years and above who reside in Riyom L.G.A since the onset of the first major ethno-religious crises in Plateau state in 2002 and who gave their consent to participate in the study. Of the 216 participants recruited for the study, only 200 completed the study. Sample size determination was done to calculate the minimum number of participants to be studied. The minimum sample size was determined using the Leslie Kish formula 22 and using a prevalence of 13.0% from a similar study done in Nigeria.23
[the standard normal deviate set at 1. 96 which corresponds to the 95% confidence level], (5%),
n=(1.962×0.13×0.87)/0.052=174
In adjusting for non- response, poor response, and incomplete response, 15% of the calculated value was added, which gave as the minimum number of participants to be recruited for the study to give the desired power and effect size subsumed in the Kish formula.
The study was approved by the Jos University Teaching Hospital’s Institutional Health Research Ethical Committee with reference number: JUTH/DCS/ADM/127/XIX/6597. Permission was obtained from the LGA chairman and the community head of the selected community. Informed consent was obtained before commencement of the study.
2.2 Measures
Details of data collection and procedure of the study have been described elsewhere in a previous study.24 Participants who gave their consent for the study but were not literate enough to append their signatures were required to thumbprint as appropriate. Comprehensive explanation of the study was proffered, respect for their rights were recounted, and confidentiality was assured for the participants. Areas were mapped and visits were made to potential participants by the five interviewers who had been trained in the administration of the questionnaires [Composite International Diagnostic Interview (CIDI),25 and the WHO quality of life questionnaire (WHOQOL-BREF)] and their scoring systems.26 Face to face interviews were carried out, the meetings were verbally done and each lasted an average of 75 minutes. Participants with depression or other psychological problems received brief psychological intervention during the study. Furthermore, severe cases identified during the study were referred to treatment centres such as Jos University Teaching Hospital and Vom Christian Hospital for subsequent management.
2.2.1 The depression module of the Composite International Diagnostic Interview (CIDI)
A structured clinical interview designed with the property of generating diagnosis according to the International Classification of Diseases 10th Revision (ICD 10) of the World Health Organization and the Diagnostic and Statistical Manual 4th Edition (DSM IV) of the American Psychiatric Association and designed for use across cultures.27,28 It was developed for people with different educational /cultural backgrounds and intelligence. The CIDI has been shown to have good validity, good test- retest reliability, inter-rater agreement, and acceptable degrees of concordance for the detection of depression and has been validated and used by researchers in different countries, Nigeria inclusive.25,29 The English and Hausa version of the WMH-CIDI were used for participants who speak English and Hausa (a language widely spoken and understood by residents of northern Nigeria) respectively.
2.2.2 WHO Quality of Life questionnaire (WHOQOL-BREF)
The WHOQOL-BREF is a 26- item questionnaire,26 which is a short version of the WHOQOL-100 scale.30 It consists of four domains: Physical Health (7 items), Psychological (6 items), Social Relationships (3 items), Environment (8 items) and Global QOL (2 items).26 The different domains in the WHOQOL-BREF encompasses different areas of daily life and provides the basis for evaluating the perception of individual’s satisfaction in relation to their objective and subjective living conditions. It is a self -rating instrument but can also be interviewer-administered. The scores can range from zero to 100, with higher scores representing better QOL. It has been shown to have excellent psychometric properties and a valid measure of QOL in the older adults.26 The WHOQOL-BREF has been vaildated and adapted for use in several Nigerian studies.31–33 The Hausa version of the WHOQOL-BREF used in this study has been used previously in studies carried out in northern Nigeria.24
2.3 Statistical analysis
The Statistical Package of Social Sciences Version 23 (SPSS-23) was used for the statistical analysis.34 Non-numeric variables such as gender, age group, occupation, marital status etc. were presented using frequency tables in frequency and percentage. Logistic regression analysis was used to determine on one hand, independent significant associations between major and sub-threshold depression, socio-demographic/risk factors, and on the other hand, to compare the difference in means of domains of QOL between presence and absence of full and sub-threshold depression. Probability value (p-value) of less than 0.05 was considered statistically significant. Adjusted odds ratio and 95% confidence interval were used as point and interval estimate respectively.
3.0 Findings
The study had a 92.6% response rate. The age range was 60-104 years and the age group 60-69 years had the highest prevalence (61.0%) compared to other age groups. Females constituted 60.0% of the study population with a male to female ratio of 0.6:1. Majority of the participants (89.0%) were farmers and over half (68.0%) of the participants had no formal education. The average monthly income of participants ranged between ₦0 to ₦20,000 ($0 to $50) (equivalent to 2USD, using the exchange rate of 400 Nigerian naira to one USD as at the time of data collection), with less than half (45.5%) earning an average monthly income of ₦800.00 ($2).
As shown in Table 2, logistic regression shows the relationship between sociodemographic/ risk factors and lifetime major and subthreshold depression. Lower monthly income, history of trauma, and having a confidant after the event had increased odds of having major depression (OR=1.839, CI=1.364–2.480, p=0.001); (OR=9.860, CI=1.025– 94.876, p=0.048); (OR=4.570, CI=1.783–11.718, p=0.002) respectively. Whereas, having someone to talk to afterwards and access to health care had increased likelihood of having subthreshold depression (OR= 5.105, CI=1.037–25.133, p=0.045); (OR=0.276, CI=0.088–0.862, p=0.027) respectively.
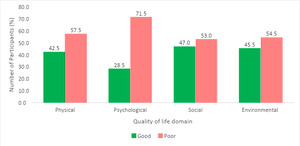
There were more participants with poor QOL than those with good QOL across the four domains as shown in below in Figure 1. The study showed that more than half (57.5%) participants had poor physical QOL. Similarly, 71.5%, 53.0% and 54.5% participants had poor psychological, social, and environmental QOL respectively.
Table 3 shows that lower mean scores were seen across the four domains for participants who were found to have poor QOL in this study. These suggest that more participants were more likely to be dissatisfied in all the QOL domains. Statistically significant differences in the mean scores of poor and good QOL were demonstrated with p=<0.001 across the domains.
As shown in Table 4 below, higher scores were seen in participants without, compared to those with depression. Significant relationships were seen in the social and environmental domains for major depression with p= <0.001 for each. Participants with major and subthreshold depression have some impairment in the social, environmental, and physical domains of QOL.
4.0 DISCUSSION
In this study, the prevalence of major depression among older persons was 58.5% and an additional 12.0% was found for subthreshold depression. The present study reported higher prevalence of depression compared to results from previous studies on late life depression in Nigeria which ranged from 1.1% to 44.7%.35,36 The observed disparity in the prevalence of late life depression in the present study in comparison to previous findings both locally and in other countries can be explained by the repeated exposure of the participants to mass violence spanning two decades, neglect and failed promises by the government to support them and bring to book the perpetrators of these massacres, inappropriate shelter, and limited access to adequate health care facilities. On the other hand, the present study was lower than the 81.1% prevalence reported in a meta-analysis by Zenebe et al with the range of 7.7% to 81.1%.1,37,38 Difference in sample size, instruments, methods, and cultural factors may have contributed to the higher prevalence recorded by Ashe et al in India.38 Comparable prevalence was seen for subthreshold depression with a range of 15% to 27% seen amongst older persons in community settings, however our finding was lower than the 53% reported in South Africa.39,40 Additionally, the use of the Geriatric Depression Scale, a screening tool may have contributed to the variations in results.
Findings from our study supports amassing evidence that both major and subthreshold depression are more common in older persons in rural settings than documented.41,42 Participants who earned N800 ($2) or less were more likely to have depression compared to those who earned more or were in the higher income groups. This is consistent with previous findings which support positive associations between low socioeconomic status and depression.43,44
All the participants in this study earned less than ₦20,400 ($51) monthly which is below the poverty line of $1.90 a day (approximately $57 per month) stipulated by the World Bank, consequently putting them in a disadvantaged position socioeconomically. Participants with lower income had a higher likelihood of depression compared to other income groups in the present study. Additionally, findings from our study show that having someone to confide in, was a common factor associated with both major depression and subthreshold depression. While a history of trauma and low income was associated with major depression; poor access to health care was associated with subthreshold depression. The experience of witnessing their homes and communities destroyed with majority of their younger populations murdered, heightened by the loss of their means of livelihood, subsequent displacement leading to their dependence on strangers and extended family for support coupled with the frustration of unavailable health services may lead to a sense of reduced relevance in the society, low self-esteem, negative view of self and the future.45,46 On the one hand, socioeconomic stability has been found to be protective against depression,43,47 having a meaningful source of income furnishes individuals with a sense of purpose and boosts self-esteem.
Depression in the geriatric population is known to be significantly associated with negative outcomes.40 QOL among the older adult is an important area of concern which reflects the health status and well-being of this vulnerable population. The QOL in this study was generally poor across all domains and these suggest that participants in this study were dissatisfied in the four domains related to QOL. This study highlighted findings that participants without depression had higher scores across the domains translating to better QOL than those with depression. Significant relationships were found with major depression in the social and environmental domains and in the physical domain for subthreshold depression. Older persons in this study reported dissatisfaction with their immediate environment viz a viz the increasing security challenges, death of their loved ones particularly as it has affected their support system worsened by the increased structural and functional deficits and emergence of medical comorbidities associated with advancing age. Furthermore, their poor living conditions, inadequate nutrition, absence of basic amenities, dilapidated health care center and the difficulty in accessing better health facilities are plausible suggestions for the significant relationships in the social, environmental, and physical domains for participants with major and subthreshold depression.
The findings above in this study are consistent with numerous studies which support the negative relationship between QOL and depression locally,19,31,32 and comparable to reports which highlights the presence of depression as an important factor in estimates of poor QOL in other countries.13,19,42,48 However, these local and international findings deviate from results by Akosile et al conducted among older persons in Nigeria where good QOL yet high prevalence of depression was reported among participants.33 Possible suggestions for the disparity in results were the use of convenience sampling technique, higher number of participants who had formal education and were gainfully employed compared to participants in the present study.
The community-based nature of this research among internally displaced older persons, an otherwise unreachable population was considered a strength. In addition, this study is one of the few studies from sub-Saharan Africa that assessed sub-threshold depression in older persons. However, this study is not without limitations. The cross-sectional nature of the survey precludes drawing up any causal relationships between depression, socio-demographic/risk factors and QOL. Participants were limited to a conflict-ridden community in Nigeria, therefore further studies may be required locally and globally to determine generalization among older persons. Furthermore, it is possible that recall bias, forgetfulness as a normal aging process and cultural factors may have led to an underestimation of depression in this study.
Conclusion
For too long, research on mental health conditions from sub-Saharan Africa among traumatised persons have focused on children and younger adults and very few have examined the effect on older persons. Moreover, sub-threshold form of depression has been overlooked among this subset of the population while emphasis has been on major depression mostly. Consequently, symptoms suggestive of this phenomenon are usually wrongly attributed to the attendant problems of aging. If not explored, they may go unnoticed or discounted. The present study highlights a high prevalence of major and subthreshold depression among traumatized older persons and substantial impairment in the domains and significant interference in the QOL of those with both major and subthreshold depression. It also underpins the need for more longitudinal research on sub-threshold depression among older persons, highlights the need for a higher index of suspicion by clinicians, the additional need to focus on improving the detection of sub-threshold depression in older persons, particularly those that have suffered traumatic events; and the potential importance of interventional studies on major and minor depression to consider risks factors identified.
Acknowledgement
The authors would like to thank the kind people of Hoss community in Riyom Local Government Area (L.G.A), the ward heads, community leaders and the chairman of Riyom L.G.A of Plateau state, Nigeria for their support and contribution to this study.
No funding was provided for this study and the authors declare no conflicting interests.
Authors’ contribution: MIO, BO, CGP, GSG, TA, RU are co-investigators and contributed to the design and draft of the study. MIO led the write up of this manuscript. MIO, and RU conceptualised the manuscript, with input from all authors. MIO, RU, BO and TA designed the study and wrote the statistical analysis plan, with input from all authors. MIO drafted the first version of the manuscript. All authors read, drafted, and critically revised the whole report. BO acts as guarantor for the manuscript.